Moira Squires was too young when she was diagnosed with aggressive triple-negative breast cancer.
She was too young to suddenly have to consider her mortality. She was too young to face leaving her husband, Eugene, and their two children, 5-year-old Keira and 7-year-old Liam, behind. But she was also too young, in the eyes of some breast cancer screening guidelines, to have a mammogram.
And so, at age 36, she found the lump herself.
“I trusted my gut,” she said during a telephone interview from her home in Southampton, “and my gut saved my life.”
As Squires endured what came next — chemotherapy, a double mastectomy, radiation therapy and reconstruction — she realized she wasn’t alone in her age bracket. There were other women navigating the same challenges she faced, from raising children in the midst of treatment to physically reconnecting with their partners, and they started gathering three years go.
They called themselves the Warriors of the East End, a place where young women — typically ranging from age 20 to 50 — can come together and talk about the issues that matter to them, whether it’s cancer or not.
“We’ve been through it and we can relate because we’re of similar age and similar situations — we’re not retired women whose children are already grown,” Squires said. “I’m sad that there’s so many young women being diagnosed, but I’m happy to provide an environment for them where we can show each other our scars and really get down to the nitty-gritty.”
Last month, the U.S. Preventative Services Task Force introduced a draft recommendation statement that would reduce the age for biannual breast cancer screenings from 50 to 40 — a move that Squires and local experts agree is a step in the right direction but not nearly enough.
“I think we have to get very almost fanatical in our passion,” said oncologist Dr. Francis Arena during a telephone interview from the Riverhead location of Perlmutter Cancer Center at NYU Langone Arena Oncology, which he founded. “This is a disease that can be cured if caught early, and anything that stops us from catching it early, we have to absolutely be irate.”
The new guidelines, which apply to women at average risk of breast cancer, is an update to the 2016 recommendation from the U.S. Preventative Services Task Force, which is an independent, nonfederal volunteer group composed of national experts in prevention and evidence-based medicine, according to its website.
It suggested biennial screening mammography for women age 50 to 74, and individualizing the decision to undergo screening for women age 40 to 49, based on factors such as individual risk and personal preferences and values.
“When they said, ‘Start at the age of 50,’ I was brokenhearted. I was furious,” recalled three-time breast cancer survivor Susie Roden, president of the Coalition for Women’s Cancers at Stony Brook Southampton Hospital and vice president of Lucia’s Angels. “So I think it’s very important that women start at the age of 40.”
According to the USPSTF, breast cancer is the second-most common cancer in women — one in eight will be diagnosed in her lifetime. Black women are at a 40 percent higher risk of dying from breast cancer, and it is estimated that this change in guidelines will save 19 percent more lives.
“New and more inclusive science about breast cancer in people younger than 50 has enabled us to expand our prior recommendation and encourage all women to get screened every other year starting at age 40,” according to a statement from Dr. Carol Mangione, the task force’s immediate past chair. “This new recommendation will help save lives and prevent more women from dying of breast cancer.”
In 2022, it is estimated that more than 280,000 women were newly diagnosed with breast cancer, and over 43,000 women were estimated to die from it. According to the National Cancer Institute, one in 28 women between age 60 and 69 will be diagnosed with breast cancer. For age 50 to 59, that drops to one in 42, followed by one in 65 between age 40 and 49, and one in 204 between age 30 and 39.
“One in 204 to one in 65, that’s a tremendous difference, and it’s a huge jump,” said Dr. Susan Lee, chief of breast surgery at Peconic Bay Medical Center. “When breast cancer is found at a younger age, they tend to be more aggressive, they’re more biologically advanced and they’re more likely to be caused by genetic mutations. As a matter of fact, in the 40 to 49 age group, breast cancer is the most common cause of nontraumatic death.”
In his practice, Arena sees breast cancer constantly — upward of 20 women every day — and many of them are “young,” he said, the vast majority over the age of 30. The youngest he’s seen was 26, he said.
“We have this unmet question of, ‘Why do so many young ladies get this?’” he said. “And the answer is, ‘I don’t know.’”
Outside of risks like simply being female, increasing age and a personal or family history with breast conditions, other factors include obesity, alcohol consumption, postmenopausal hormone therapy — which is less common today — a menstrual cycle starting under age 12, women having their first child after age 30, and never having been pregnant.
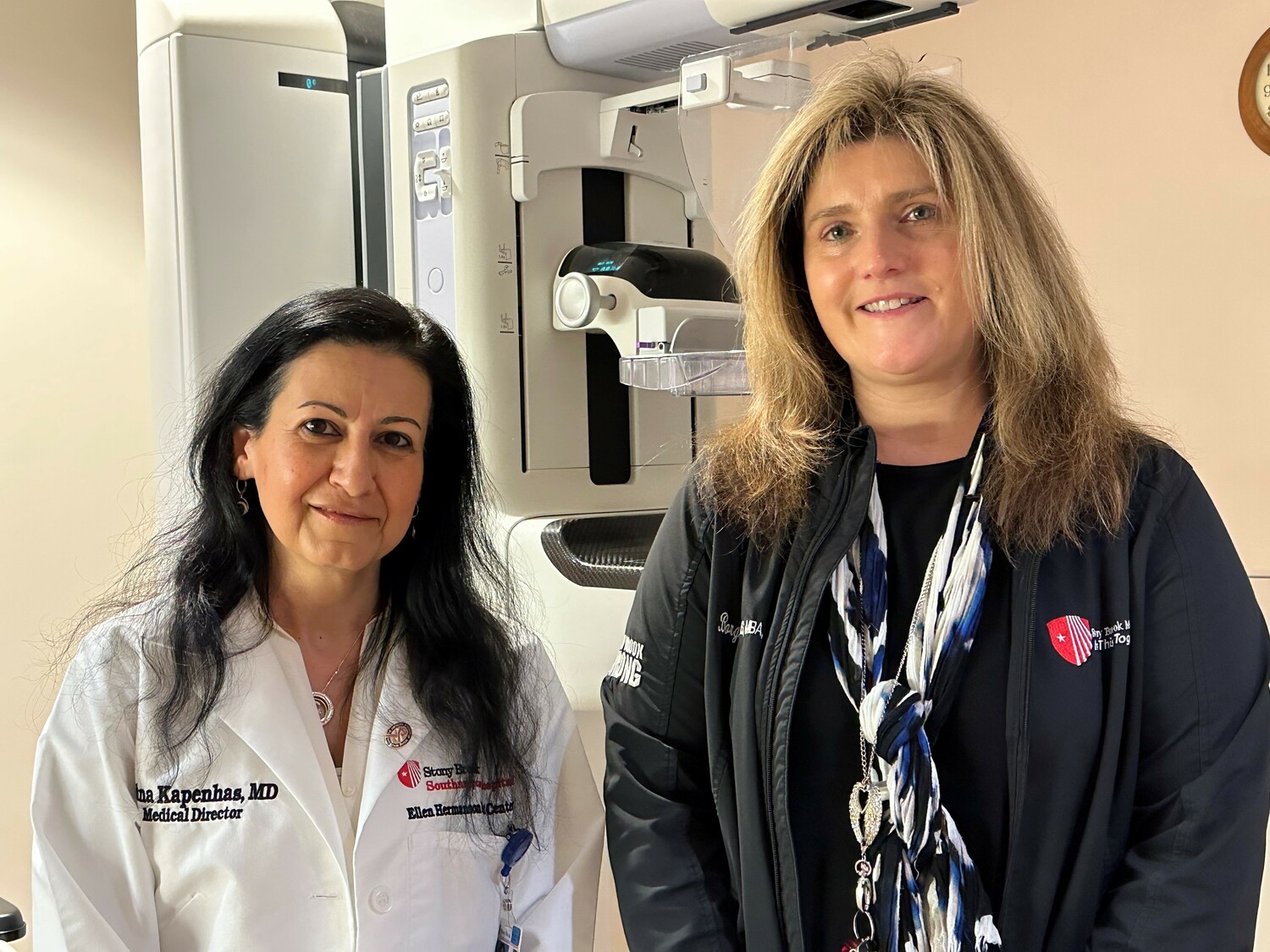
But for some women, none of these apply, which is why foundations like the American College of Radiology and American Society of Breast Surgeons have urged mammography starting at age 40 all along, as have other local institutions, including Stony Brook Southampton Hospital, according to Dr. Edna Kapenhas, head of breast surgical oncology there and medical director of the Ellen Hermanson Breast Center.
“We know if you start screening at age 40 and you get an annual mammogram, it has been shown time and time again that it does save lives,” she said. “Even though the task force recommends every other year, we will continue to advise our patients and our community to get a mammogram every single year starting at age 40.”
Lee, who also recommends risk assessments starting at age 25 or 30, said that lead time — or the amount of time that it may take cancer to develop — is less in younger people, about 1.7 years. The other experts agreed, noting that they will still advise their patients to get annual mammograms and to adjust the starting age if risks are present.
“Our stakes here is a woman’s life,” Arena said. “We’re not talking about something that is pedestrian, we’re talking about something that is intrinsic, that needs to be protected, and we need to give all the opportunities that are necessary and not just put on these rigid guidelines — because they’re going to be interpreted by the insurance companies as mandates that they don’t have to give service, and that’s wrong.”
In New York, Shannon’s Law — named after Shannon Saturno, a third grade special education teacher in Babylon who died from triple-negative breast cancer at age 31 — requires large group insurers to cover mammograms for women age 35 to 39. But some insurance carriers across the nation do not cover the cost until age 40, or take advantage of loopholes, Arena said.
“Sometimes the most vulnerable are those that are under-served — and, let me tell you, we have to help,” he said. “I don’t care what race, creed, color, ethnicity, religious beliefs — I’m there. We all have to be there. We have to realize that we need to protect these young people and we can’t have bullies, such as insurance companies who want to make a profit for their stockholders, be the ones that are controlling the day.
“We control the day,” he continued. “We control the data. We can see what’s going on. No one’s gonna pull the wool over our eyes. No way.”
At the Ellen Hermanson Breast Center, any patient who is under-insured, noninsured or undocumented is covered, explained Director Laura Borghardt, who is director of the Phillips Family Cancer Center and director of cancer services at Stony Brook Southampton Hospital.
“It’s one of the things that we offer our patients here, if anyone’s ever struggling, to make sure that that is not something they need to worry about on top of a cancer diagnosis,” she said.
Earlier this month, public comments closed for the task force’s draft recommendations, which they will consider as the final recommendation is developed. And while it will not likely impact health care on the East End, it will affect hospitals and providers across the country that only encourage screenings for women age 50 and older.
“It’s really, really great to know that other places throughout the United States are gonna be also doing this and hopefully, they’re gonna see the same thing that we are,” Borghardt said, “that we’re able to catch and cure cancer sooner for these patients.”
For an hour and a half on the last Friday of most months, between five and 10 young cancer survivors gather at the Southampton Firehouse over charcuterie, sparkling water and wine — for those who partake — and talk about their lives, from the mundane to the more serious.
Inevitably, their cancer stories come up. Sometimes it’s light-hearted, Squires said, sometimes it’s not, and the group meets them with open arms. They’ve shown each other their scars, both physical and emotional, and they’ve shared their experiences. In talking and listening, they’ve started to heal with time.
“My survivor sisters get it. They get it,” explained Squires, who is an ICU nurse at Stony Brook Southampton Hospital. “I don’t know what I would do without them in my corner, in my life. It’s just vital to me.”
On Thursday, June 22, Squires celebrated her 44th birthday, seven years cancer free. And her husband and their children, who are now 12 and 15, watched as she beat the odds, finding purpose in her journey through helping others who now face what she did.
“Of course, I had days where I wanted to give up and give in to the dark. It was hard. It was really challenging,” she said, adding, “I just remember looking at my kids and thinking, ‘Oh my God, they’re so young. What are they gonna do without me and how am I going to do this?’”
She paused. “But then I was like, ‘Okay, you know what? I have to do this. I have to fight. And I have to face this battle to be here and to win and to live because they need me. My husband needs me.’ They were the reason that I pushed through.”
For more information about The Phillips Family Cancer Center’s Warriors of the East End gathering, or to join, contact Moira Squires at morose79@yahoo.com.